Successful clinical results using Obsidian® RFT in complex anal fistula treatment
Retrospective study of 80 patients presented at ECC 2025
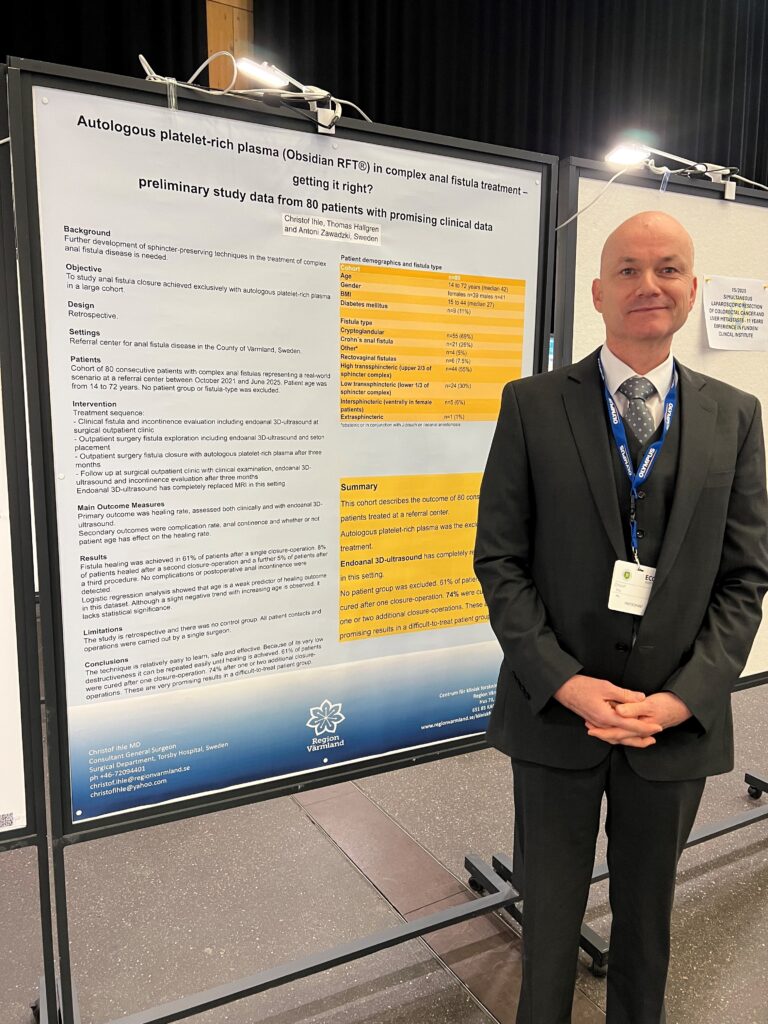
At the 2025 European Colorectal Congress (ECC) in St. Gallen, Switzerland, new clinical data were presented demonstrating the potential of Obsidian® RFT (regenerative fistula treatment), Vivostat’s autologous platelet-rich fibrin technology, in the treatment of complex anal fistulas—a condition known for its challenging nature, high recurrence rates, and substantial impact on patient quality of life.
The study, led by Dr. Christof Ihle from the Surgical Department at Torsby Hospital, Region Värmland (Sweden), evaluated the outcomes of 80 consecutive patients treated exclusively with Obsidian® RFT.
Study overview
The retrospective cohort included patients aged 14–72 years with diverse fistula types and etiologies, including cryptoglandular and Crohn’s-related fistulas. No patient group was excluded, creating a representative and clinically relevant dataset.
Clinical workflow included:
- Comprehensive fistula assessment and continence evaluation
- Fistula exploration and seton placement
- Closure using autologous platelet-rich fibrin (Obsidian® RFT)
- Follow-up with endoanal 3D ultrasound and clinical examination
Notably, endoanal 3D ultrasound fully replaced MRI throughout all stages of diagnosis, intervention planning, and post-treatment assessment.
Key results
The study findings highlight the promise of Obsidian® RFT as a minimally destructive and repeatable treatment option for complex anal fistulas:
Healing outcomes
- 61% achieved fistula healing after a single Obsidian® RFT closure procedure
- 74% achieved healing after up to two additional repeat procedures
- Healing was documented both clinically and through endoanal 3D ultrasound
Safety profile
- No complications were observed
- No postoperative incontinence was reported
- The procedure was well-tolerated across all patient subgroups
Patient and fistula diversity
- Included high and low transsphincteric, intersphincteric, extrasphincteric, and rectovaginal fistulas
- Included both cryptoglandular and Crohn’s disease–associated cases
- BMI, gender, diabetes and age variation did not preclude treatment
Logistic regression analysis indicated that age showed no statistically significant effect on healing outcome, although a slight negative trend was noted in older patients.
Clinical significance
Complex anal fistulas often require treatment strategies that balance efficacy with preservation of sphincter integrity. Many existing surgical options carry a risk of recurrence or incontinence.
The data presented by Dr. Ihle suggest that Obsidian® RFT offers several important advantages:
- Tissue-preserving: the technique avoids sphincter damage
- Repeatable: additional applications can be performed safely
- Simple to learn: procedure can be adopted by colorectal surgeons with ease
- Applicable to all fistula types: inclusive of complex, high and Crohn’s-related fistulas
These characteristics make Obsidian® RFT a valuable addition to the therapeutic arsenal for this difficult-to-treat condition.
Acknowledgment
We extend our sincere thanks to Dr. Christof Ihle and the surgical team at Torsby Hospital for their continued dedication and for sharing this important clinical evaluation with the wider medical community. Their work contributes meaningfully to the advancement of safe, regenerative, and patient-centered solutions in colorectal surgery.
